The partial thickness trabeculectomy
(trab) was first described by Cairns1 in 1968 and still remains the
gold standard in the patients who fail to have their intraocular pressure (IOP)
controlled on maximal medical therapy. Although success of trab has increased
with the use of topical mitomycin-C (MMC) as an adjunctive therapy since its
first use by Chen et al,2 its failure rate is still significant
ranging from 20 50% with long standing followup.3-6 The primary
reason for long term failure is due toepiscleral fibrosis or conjunctival
thickening overlying the area of filtration. This process of wound healing and
tissue remodeling continues to occur indefinitely after the initial surgery.
The failure of trab with flat filtration bleb and raised IOP therefore requires
several options such as addition of medical therapy, repeat trab, drainage
implants, revision of existing bleb and cyclo-destructive procedures.
Needle
revision of failing drainage bleb is performed to separate and lyse the fibrous
tissue bands in the scleral flap and inconjunctival bleb, to increase the
surface area for filtration. It was first described by Mardelliet al7
in 1996 and is subsequently popularized by other workers.8-11 The
procedure can be performed at the slit lamp or in the operating theatre. The
technique involves external revision, internal revision via anterior chamber
(AC), with or without anti-fibrotic agents.
We performed needle revision of failed
filtering blebs with adjunctive use of MMC in cohort of patients who presented
in glaucoma clinic with IOP of >25 mmHg. The purpose of our study was to
assess the outcome of needle revision with regard to decrease in IOP of < 20
mmHg with mean follow up of one year and to observe the complications associated
with the procedure.
MATERIAL AND METHODS
This study is retrospective, non-comparative,
interventional case series of 46 eyes (46 patients), who presented with IOP of
>25 mmHg after going under Trab at Isra Postgraduate Institute of
Ophthalmology and Aga Khan University Hospital, Karachi, due to initial
diagnosis of Primary open angle glaucoma (POAG) or Primary angle closure
glaucoma (PACG). All surgeries were performed earlier with the adjunctive use
of MMC. A total of 61 eyes of 61 patients had needle revision from January 2007
to December 2010. All needle revisions were performed from 2 weeks to 1 year
post trabeculectomy. All patients had argon laser suture lysis before needle
revision and were naοve to any anti-glaucoma medication. Patients with repeated
Trab and other glaucoma procedures were excluded from the study. Fifteen
patients were lost to the follow up or had follow up of < 6 months which
were not included in the study. Gender distribution showed 34 male and 12
female patients. Patients age ranged between 47 to 72 years with median age of
58 years.
Technique
Conjunctiva was anesthetized with several drops of Proparacaine
0.5% (Alcaine Alcon, Belgium), followed by one drop of 5% Povidone-iodine.
Two percent Lignocaine (0.1ml) and MMC in concentration of 0.2mg/ml (0.1ml) was
drawn into tuberculin syringe with 27 gauge needle and was given
subconjunctivally in the superior fornix above the bleb (Fig. 1 and 2). Closed
eye massage was done to diffuse the given solution (Fig. 3). Patient was
positioned on the slit lamp and wired speculum was placed to open the eye lids.
A tuberculin syringe with 27 gauge was introduced under the conjunctiva as far
away as possible from bleb and advanced to the scleral flap. With slow motion
all the adhesions between conjunctiva and episclera were separated. The needle
was further introduced under the scleral flap and with side motions episcleral adhesions
are broken down (Fig. 4). In the pseudophakic patients, needle was advanced
through the internal osteum into the anterior chamber. Once the bleb is
reformed, needle was gently removed (Fig. 5).
The IOP was rechecked postoperatively and patients
were commenced on topical Moxifloxacin 0.5% (Vigamox Alcon, Belgium), 1 drop
4 times a day for 1 week and Dexamethasone 0.1% (Maxidex Alcon, Belgium), 1
drop 4 times a day for 4 weeks. Patients were followed at day 1, 1 week, 1
month and at 3 months subsequently. Mean follow up of all patients was up to 13
months (range 6 18 months).
The successful outcome of the needle revision was
defined as IOP between 6 mmHg to 20 mmHg without any anti-glaucoma medication.
All immediate and post-operative complications were recorded.
The data analysis was carried out on SPSS for
windows version 17. A p-value of < 0.05 was consi-dered statistically
significant. The base line and follow up IOPs were compared with paired sample
T test.
RESULTS
Twenty six patients (26 eyes) out of 46 patients (46
eyes) showed improvement in IOP of < 20 mmHg, achieving success at 57%. The
pre-operative mean IOP of our patients was 26.7 ± 6 mmHg(95% Confidence
Interval 25.16 28.23), while post-operative mean IOP was 13.5 ± 4 mmHg (95%
Confidence Interval 12.47 14.5) at the mean follow up of 1 year.
All patients had small areas of subconjunctival
hemorrhage at the point of entry of needle. Transient hyphema was noticed in 1
(2.17%) patient and 2 (4.34%) patients went into hypotony with IOP of < 6
mmHg. All these eyes resolved spontaneously with no additional treatment.
The risk factors for failure to achieve IOP of <
20 mmHg in our series was pseudophakia, female gender and needle revision
carried out within one month of trabeculectomy.
DISCUSSION
Needle revision of the failed drainage bleb after
trabeculectomy, offers several advantages over repeat trab or insertion of
setons. It is a simple technique, which can be performed on the slit lamp in
the examination room on outpatient basis. It spares conjunctiva from any trauma
to make it suitable for any repeat procedure and it also reduces the cost of
the Operating theatre.
The success rate of this procedure in our series of
46 patients was at 57%, reducing IOP to <20 mmHgin 23 patients. One of our
patients developed hyphema (2.17%) and two (4.34%) went into hypotony
post-operatively. In Mardellis series published in 19967, 62 eyes
were reported for bleb needle revision. Although he achieved 75.8% success in
reducing IOP of < 18 mmHg, there were averagely 2 needling procedures performed
per patient.

Fig. 1: Entry of needle subconjunctivally
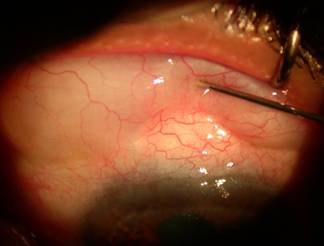
Fig. 2: Injection of lignocaine with MMC
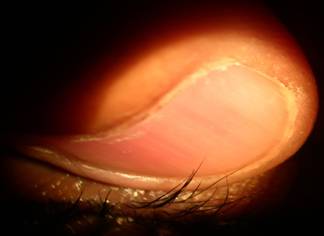
Fig. 3: Closed lid massage

Fig. 4: Cutting of adhesions
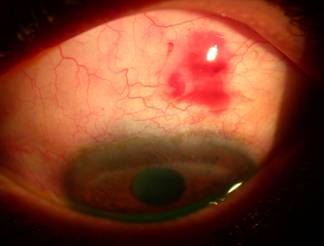
Fig. 5: Formation of bleb
He also used 0.03ml of mixture of 0.004mg of MMC
mixed with bupivacaine 0.75% with epinephrine. Ten eyes developed choroidal
detachment, one eye had suprachoroidal hemorrhage, 5 eyes had bleb leaks and 2
eyes developed hyphema. Shetty and coworkers11 carried out similar
procedure in 44 patients and reported 64% of their patients achieving IOP
between 4 to 22 mmHg. However they also included patients in their successful
outcome who either had repeated needling or required anti glaucoma medication.
They also used MMC at higher concentration of 0.4 mg/ml. The complications in
their study includedhypotony (2 eyes), hyphema (5 eyes) and bleb leak (1 eye),
all resolving within couple of weeks. Pasternack12 in consecutive
bleb revision of 77 eyes, reported 52% patients achieving
IOP of 11.3 ± 3 mmHg at the mean follow up of 29.6 ± 14.4 months. However,
subconjuctival 5 fluorouracil (5FU) was used as an antifibrotic agent. Only 2
eyes developed suprachoroidal hemorrhage and 1 eye developed kissing choroidals
requiring surgical drainage in their series. The risk factors for failure in
their patients included previous argon laser trabeculoplasty (ALT), number of
previous surgeries, previous combined phaco-trab and previous use of MMC. Shin
et al13using 5-FU with needle revision reported 45% success rate at
the end of 1 year in cohort of 64 patients. Their study suggested that, use of
MMC in initial trab increased the success rate in revision. Greenfield et al14
reported outcome of needle revision in 63 eyes with MMC. They also injected
5-FU subconjunctivally in inferior fornix with number of injections, depending
upon the degree of inflammation. The overall success rate was achieved at 78%
(IOP < 22 mmHg) with or without anti-glaucoma medication at 12 months.
The direct comparison of various studies on needle
revision, reported in literature is difficult, given the different
demographics, type of glaucoma, severity of glaucoma, timing of needle
revision, varying quantity and concentration of MMC and type of anti-fibrotic
agent used.
There is limitation of our study due to its
retrospective nature, lack of control and a small sample size. Fifteen of our
patients had inadequate follow up or were lost to the follow up, which may have
influenced the final outcome. With the remaining 46 patients, fulfilling our
criteria of inclusion, it has been showed that by carrying out a simple
procedure, we can achieve an IOP of < 20 mmHg in more than 50% of patients,
avoiding any further surgery.
CONCLUSION
Needle revision of drainage blebs with MMC can
revive failed filtration procedure in at least half of the cases, avoiding
invasive repeat surgery or commencing patients again on anti-glaucoma therapy.
Authors Affiliation
Prof.
P. S. Mahar
Aga Khan University Hospital
Karachi
Dr. A.
Sami Memon
Isra Postgraduate Institute of
Ophthalmology
Karachi
Dr. Israr
A. Bhutto
Isra Postgraduate Institute of
Ophthalmology
Karachi
Dr. Dilshad
A. Laghari
Isra Postgraduate Institute of
Ophthalmology
Karachi
REFERENCES
1.
Cairns JE.
Trabeculectomy-preliminary report of a new method. Am J Ophthalmol. 1968; 5: 673-7.
2.
Chen C, Huang H, Bair J, Lee C. Trabeculectomy with simultaneous topical application
of mitomycin-C in refractory glaucoma. J Ocul Pharmacol. 1990; 6: 175-82.
3.
Palmer SS. Mitomycin as adjunct
chemotherapy with trabeculectomy. Ophthalmology. 1991; 98: 317-21.
4.
Stone RT, Herndon LW, Allinghan RR, Shield MB. Results of trabeculectomy with 0.3ml / mitomycin-C
titrating exposure times based on risk factor for failure. J Glaucoma. 1998; 7:
39-44.
5.
Singh K, Mehta K, Shaikh N. Trabeculectomy with intraoperative mitomycin-C
versus fluorouracil. Prospective randomized clinical trial. Ophthalmology.
2000; 107: 2305-9.
6.
Fontana H, Nouri-Madhavi K, Lumba J, Ralli N, Caprioli J. Trabeculectomy with mitomycin-C.
Outcomes and risk factors for failure in phakic open-angle glaucoma.
Ophthalmology. 2006; 113: 930-6.
7.
Mardelli PG, Lederer CM Jr, Murray PL. Slit lamp needle revision of failed
filtering blebs using mitomycin-C. Ophthalmology. 1996; 103: 1946-55.
8.
Greenfield DS, Miller MP, Suner IJ. Needle elevation of the scleral flap
for failing filtration blebs after trabeculectomy with mitomycin-C. Am J Ophthalmol.
1996; 122: 195-204.
9.
Ben-Simon GJ, Glovinsky Y. Needle revision of failed filtering blebs augmented
with subconjunctival injection of mitomycin-C. Ophthalmic Surg Lasers Imaging. 2003;
34: 94-9.
10. Broadway DC, Bloom PA,
Bunce C.
Needle revision of failing and failed trabeculectomy blebs with adjunctive
5-fluorouracil: survival analysis. Ophthalmology. 2004; 111: 665-73.
11. Shetty RK, Wartluft L,
Moster MR, Ibraham D.
Slit-lamp needle revision of failed filtering blebs using high-dose
mitomycin-C. J Glaucoma. 2005; 14: 52-6.
12. Pasternack JJ, Wand M,
Shields MB, Ibraham D. Needle
revision of failed filtering blebs using 5-fluorouracil and a combined
Ab-externo and Ab-interno approach. Glaucoma 2005; 14: 47-51.
13. Shin DH, Kim YY. Risk factors for failure of 5-fluorourcil needling revision for
failed conjunctival filtration blebs. Am J Ophthalmol. 2001; 132: 875-880.
14. Greenfield DS, Miller MP. Needle elevation of the scleral flap
for failing filtration blebs after trabeculectomy with mitomycin-C. Am J
Ophthalmol. 1996; 122: 195-204.